Migraines: A Quick Guide
Quick topic discussion on migraine, pathophysiology, and tables regarding medication treatment options (for acute and preventative management).
Hi everyone! Welcome back to another clinical pharmacy topic for your Wednesday morning. To be honest, my thoughts have been consumed by HIV and Opportunistic Infection topics recently. This is to be expected as my new position is specifically HIV/ID, but I usually have a topic-switch ready for my RxTeach posts!
Since I have had no such switch yet, I went to the archives of my PGY1 projects. I presented a topic discussion on Migraines in October 2021. Lucky for you, pharmaceutical therapy doesn't change too often in this disease state. When I gave this topic discussion, I had a fun "headbands" game associated with it. Unfortunately for you, we cannot play headbands through email.
Ok enough rambling. Let's jump into this brief topic!

Definition
An episodic disorder of disabling headaches generally associated with nausea and/or phonophobia and photophobia
Epidemiology
- Affects 12-15% of the population
- Women (17%) > men (6%) annually
- 30-39 years old
- Migraine without aura (75%)
- Major cause of disability
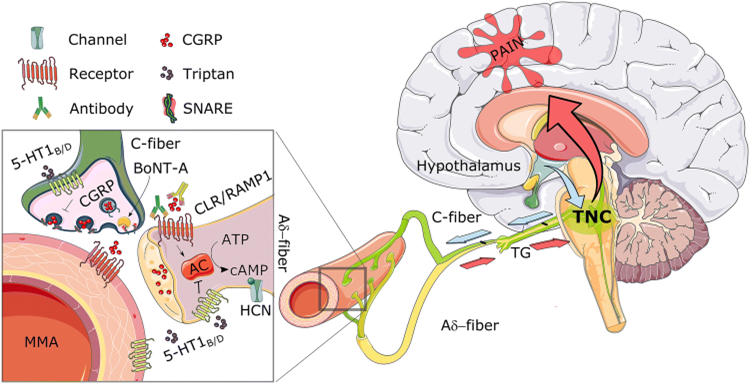
Pathophysiology - Signaling
- Activation of the trigeminovascular system
- First-order sensory neurons
- Originate in trigeminal ganglion
- Afferent fibers innervate meninges and vessels
- Dilation of dural blood vessels
- Convergence of nerve roots at spinal trigeminal nucleus in the brain stem
- Innervates anterior and posterior regions of head and neck
- Brain stem fibers trigger second-order trigeminovascular neurons in the cervical spine
- Third-order neurons activated in the thalamus + superior salivatory nucleus (SSN)
- Thalamus sends signals to sensory corte
- Perception migraine
- SSN sends signals to dural blood vessels
- Further vasodilation
- Perception of migraine
Pathophysiology – Neuropeptides and hormones
- Stimulation of the trigeminal ganglion results in vasoactive neuropeptides
- Substance P
- Calcitonin gene-related peptide (CGRP)
- Neurokinin A
- Vasodilation and plasma protein extravasation
- Elevated vasoactive neuropeptides have been found in the CSF with chronic migraine. This chronic neurogenic inflammation may lead to process of sensitization
- Sensitization is when the neurons become increasing responsive to nociceptive and non-nociceptive stimulation
- Serotonin
- Role in generation of migraine is unclear; it is known that it plays a role in the acute treatment, as we will discuss later with our treatment options, but researchers are still unsure of the direct mechanism
- Suggested that serotonin has direct action upon the cranial vasculature in central pain control pathways or by cerebral cortical projections of brainstem serotonergic nuclei
- The thought that serotonin has a role in migraine is backed by the fact that TCAs which are nonspecific in binding help decrease migraine pain but more selective SSRIs are not as effective.
- CGRP
- Appears to mediate trigeminovascular pain transmission from intracranial vessels to the CNS as is vasodilatory component of the neurogenic inflammation
- Stimulation of the trigeminal ganglion induces the release of CGRP
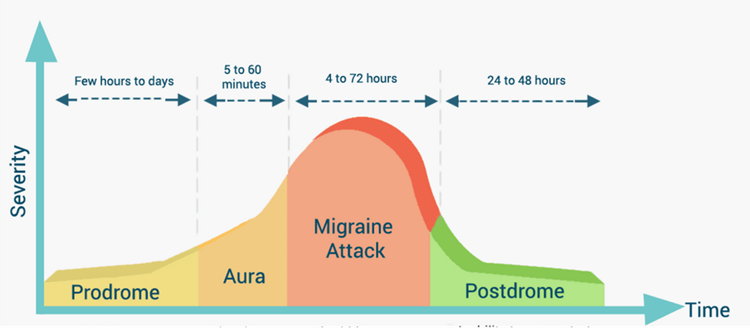
Stages of a Migraine
Prodrome: occurs up to 77 percent of migraineurs
- Yawning, euphoria, depression, irritability, food cravings, constipation, neck stiffness
Aura: about 25% of individuals
- Positive symptoms: visual, auditory, somatosensory (pain or burning), motor
Negative: absence or loss of function (opposite of the positives)
Migraine headache: unilateral, throbbing, or pulsatile, intensity increases. N/V, photophobia or phonophobia
Migraine postdrome: sudden head movements cause pain or patients feel drained, exhausted, sometimes elation or euphoria
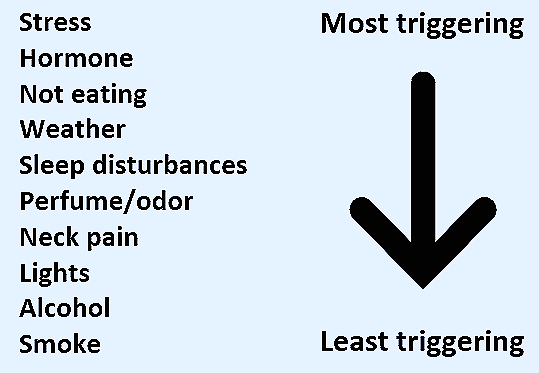
Triggers
Diagnosis (ICHD-3 criteria)
- Migraine without aura
- 5 attacks with:
- 4–72-hour duration
- Characteristics of migraine
- Phono/photophobia, N/V
- Migraine with aura
- The above + aura symptoms
Aura characteristics
A. At least two attacks fulfilling criterion B and C
B. One or more of the following fully reversible aura symptoms:
- Visual
- Sensory
- Speech and/or language
- Motor
- Brainstem
- Retinal
C. At least three of the following characteristics:
- Two or more symptoms occur in succession
- Each individual aura symptom lasts 5 to 60 minutes
- At least one aura symptom is unilateral
- At least one aura symptom is positive
- The aura is accompanied, or followed within 60 minutes, by headache
Treatment
- Avoid triggers (sounds obvious, right?)
- Beware of medication overuse headache which is from regular overuse of medications for migraine by patients who have at least 15 days per month with headache (to treat medication overuse headache, you withdraw the offending med – yes, stop the treatment medication – and start a new preventive agent)
- Story time! I had a patient who came to clinic with crazy migraine history and we were her last hope. She was on every medication listed in the guidelines and had tried every remedy imagineable. My preceptor did not want to switch around her psychiatric medications too much, but ended up removing a few after reaching out to the psychologist. Upon removing some of the medications, her relentless migraines resolved!
- Non-pharm options
- Modest evidence: noninvasive neuromodulator devices, biobehavioral therapies, acupuncture
- Little/no evidence: physical therapy, chiropractic manipulation, dietary approaches
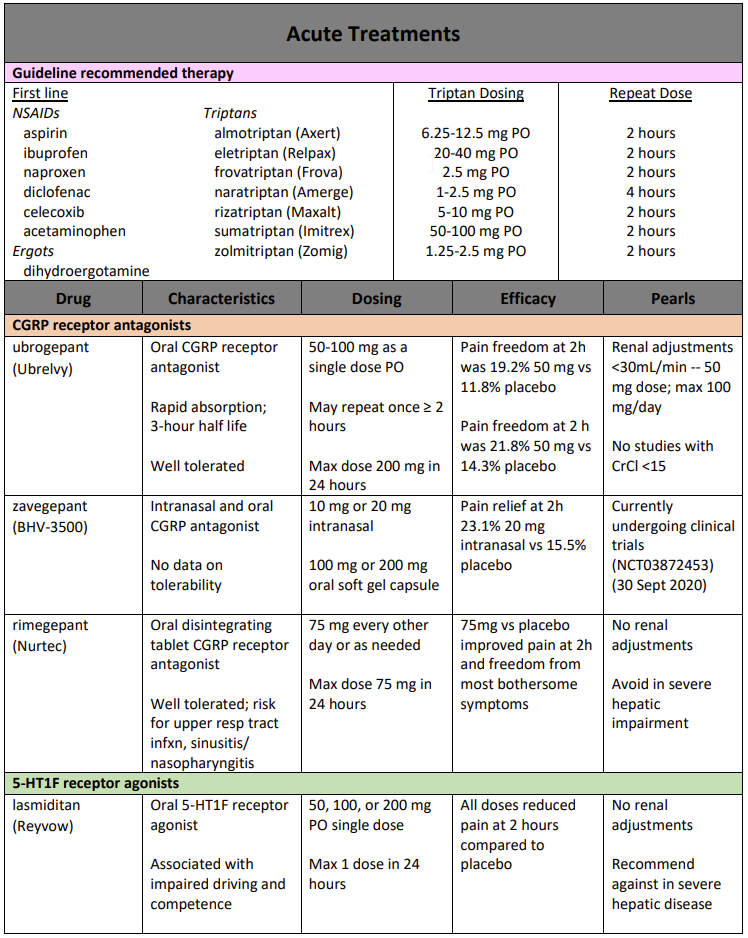
- Triptan pearls
- Take triptans EARLY in the headache cycle (when you notice premonitory symptoms or aura because once cutaneous allodynia hits it is too late
- Switch from one to another or different route if oral does not work; switch if three migraine attacks have been treated without effect
- Can do a combo of NSAID and triptan
- 5-HT1F receptor agonists
- Mechanism of agonists: agonizes the 5-HT1F receptor to decrease the expression of c-Fos, a neural activation marker, in the caudate nucleus of the trigeminum, without having any vascular effects
- Calcitonin gene-related peptide (CGRP) Receptor Antagonists
- CGRP is released from trigeminal ganglia neurons
- Transcription increases under conditions imitating neurogenic inflammation
- Activation of receptors regulates increase of cAMP and cGMP to induce vasodilation
- CGRP also stimulates production of nitric oxide (NO)
- This leads to more cGMP and vascular relaxation
- Mechanism of antagonists: inhibit CGRP transcription and reduce CGRP release
- Preventive therapies
- Aim to lower the frequency, intensity, and duration of migraine headaches
- Effective when one of the following conditions occurs
- 50% reduction in frequency of migraine days
- Significant reduction in migraine attacks or their severity or an increased response to therapeutic treatment
- A reduction in disability due to the disease
- Improvement in QOL
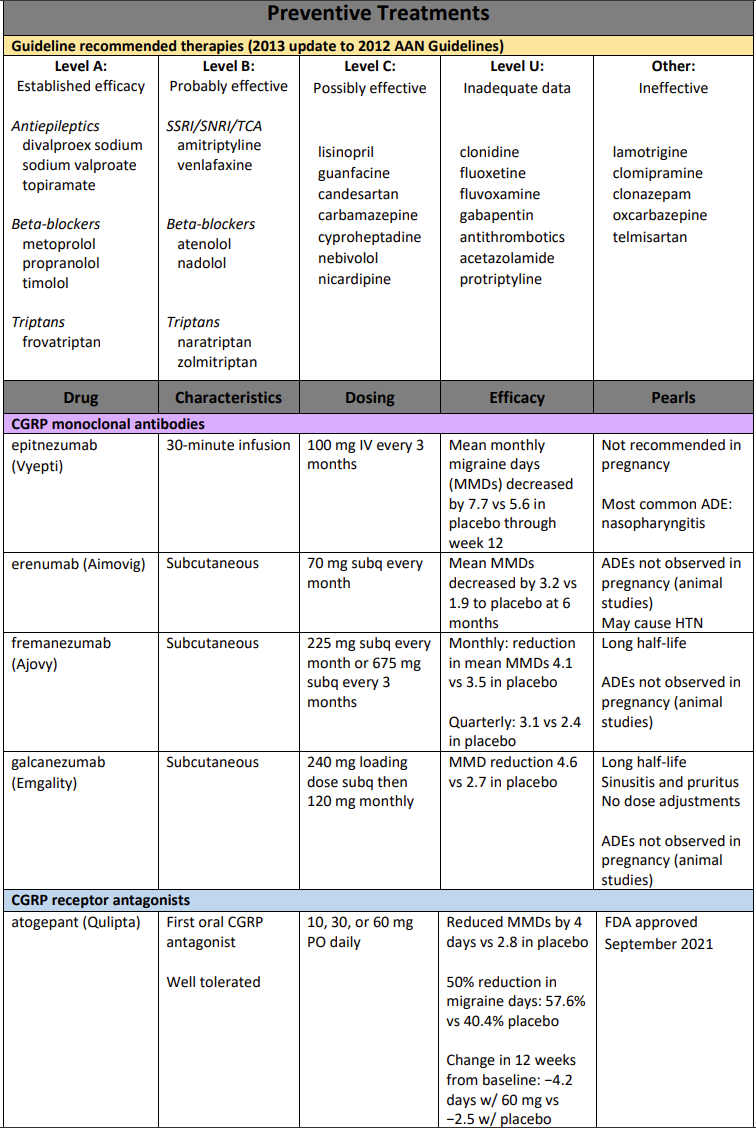
Note: all CGRP monoclonal antibodies carry hypersensitivity and injection site reaction risk.
References
- Ashina M. Migraine. New England Journal of Medicine. 2020;383(19):1866-1876.
- Burstein R, Noseda R, Borsook D. Migraine: Multiple Processes, Complex Pathophysiology. J Neurosci. 2015;35(17):6619-6629.
- Capi M, De Angelis V, De Bernardini D, et al. CGRP Receptor Antagonists and 5-HT1F Receptor Agonist in the Treatment of Migraine. J Clin Med. 2021;10(7):1429.
- Lexicomp Online, Lexi-Drugs Online. Waltham, MA: UpToDate, Inc.; July 30, 2021. https://online.lexi.com. Accessed September 29, 2021.
- Silberstein SD. Evidence-based guideline update: Pharmacologic treatment for episodic migraine prevention in adults. Published online 2012:12.
- Ailani J, Burch RC, Robbins MS; the Board of Directors of the American Headache Society. The American Headache Society Consensus Statement: Update on integrating new migraine treatments into clinical practice. Headache. 2021; 61: 1021–1039. https://doi.org/10.1111/head.14153.
*Information presented on RxTeach does not represent the opinion of any specific company, organization, or team other than the authors themselves. No patient-provider relationship is created.

