Arrhythmias
Our hearts are incredible organs, but what happens when abnormal rhythms start to take over? Dr. Liang is here to teach us all about arrhythmias and how to treat them!

Author: Feiran Liang, PharmD
Editor: Kristen Lindauer, PharmD, BCPS
We have a special edition for you this week! Dr. Feiran Liang, a current PGY1 resident at Sentara Norfolk General Hospital, recently presented a topic discussion on arrhythmias. Today we are going to dive right into the information she presented and become experts!
Dr. Liang's full PowerPoint presentation will be available to paid subscribers only. Her PowerPoint contains her slide notes, educational graphics, and references. To access, click on the “Subscribe” button on our homepage and select the tier you would like to subscribe to for premium RxTeach content!
Let’s get into the topic!
The Cardiac Conduction Pathway
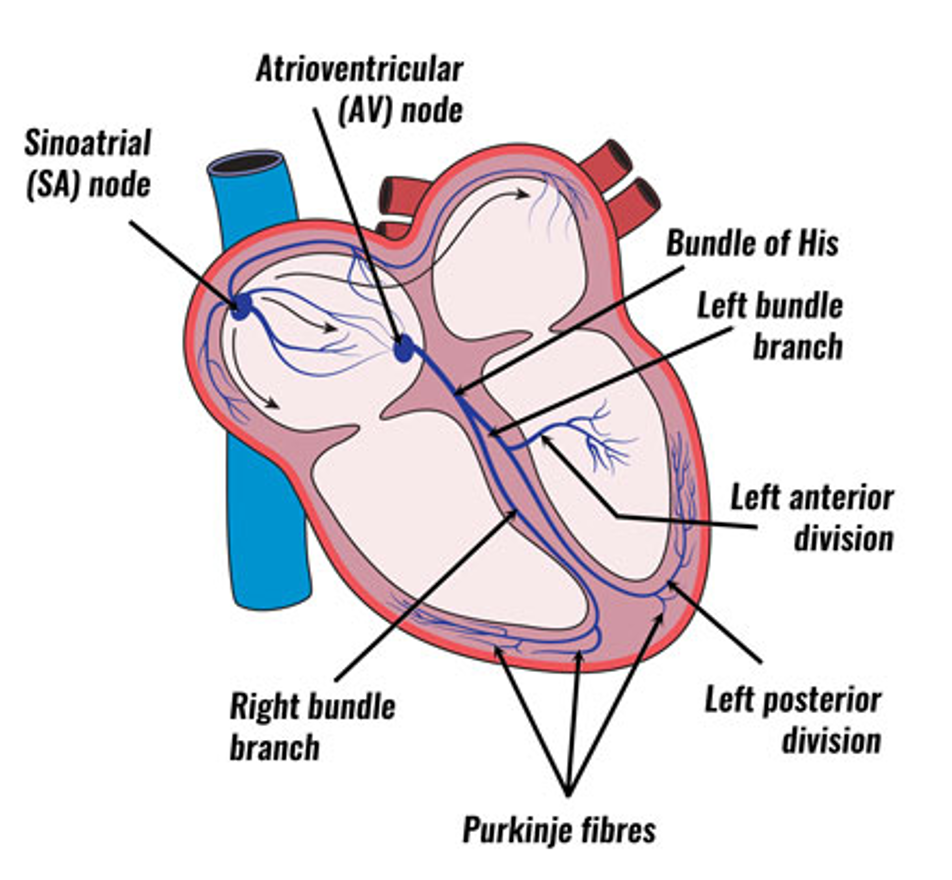
First, we need to understand how the heart functions. The heart is composed of specialized cardiac cells that send electrical impulses throughout the heart muscle. This causes our heart to contract, or "beat."
The conduction pathway begins in the sinoatrial (SA) node, travels to the right and left atria for atrial contraction, continues to the atrioventricular (AV) node, through the Bundle Of His, across the ventricles, divides into the right and left bundle branches, and finally spreads to the Purkinje Fibres for ventricle contraction. Figure 1 below provides a visual representation of the pathway!
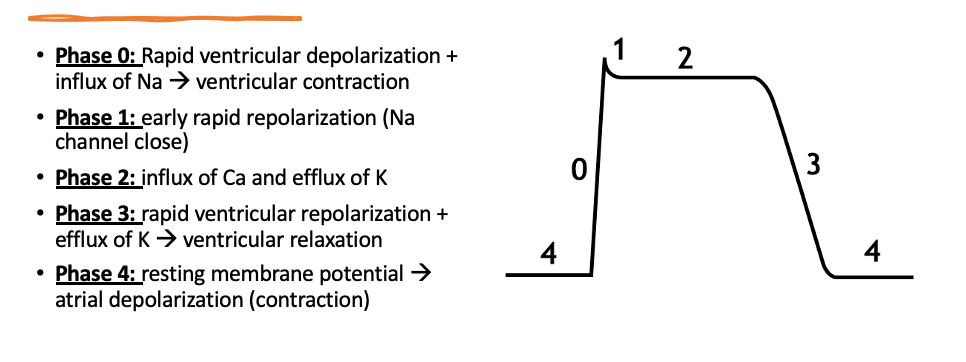
Along with the conduction pathway, we also need to understand the Cardiac Action Potential. The action potential coordinates with the movement of ions through channels in the myocytes (heart cells). Each action potential provides the electricity needed to begin the Cardiac Conduction Pathway.
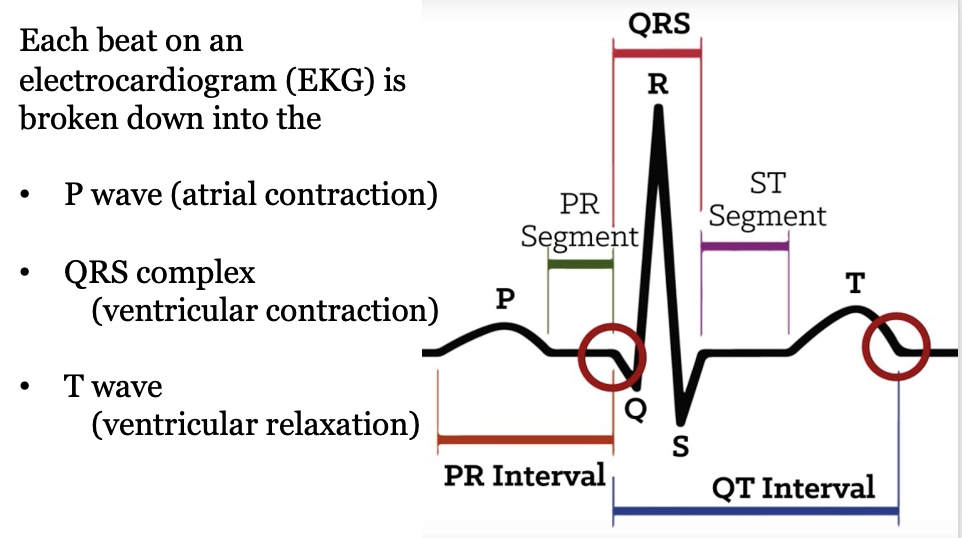
Let's Get into a Rhythm
The topic today is "arrhythmias," which refers to abnormal rhythms in the heart. What, then, is a normal rhythm?
Normal Sinus Rhythm (NSR) is what you commonly see in medical shows such as Scrubs, Grey's Anatomy, The Good Doctor, etc. (well, until something goes drastically wrong. Hang tight, we will get there!). NSR looks like this:
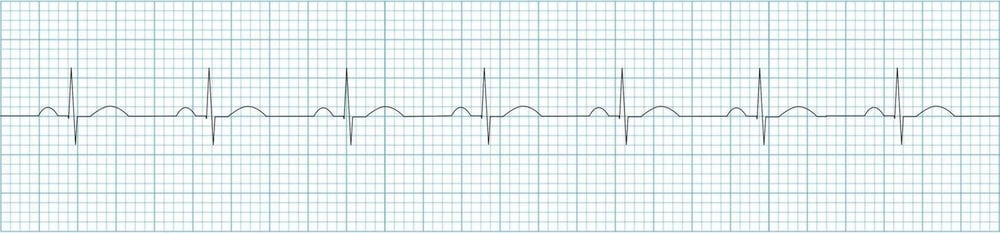
A normal heart rate is 60-100 beats per minute (BPM).
Now that we are familiar with NSR, we can jump right into the various abnormal rhythms that can occur in our patients!
Types of Arrhythmias
The easiest way to digest the different arrhythmias is to break them down into three categories as seen below. I will number the 7 different arrhythmias to help stay organized as we discuss each one in detail. Please refer to the full PowerPoint for extra details on each arrhythmia!
Sinus Rhythm
- Sinus Bradycardia (slow heart rate)
- Sinus Tachycardia (fast heart rate)
Supraventricular Arrhythmias
- Atrial Flutter
- Atrial Fibrillation (A-Fib)
- Paroxysmal Supraventricular Tachycardia (PSVT)
Ventricular Arrhythmias
- Ventricular Tachycardia (V-Tach)
- Ventricular Fibrillation (V-Fib)
Signs and Symptoms of Arrhythmias
- Dizziness
- Shortness of breath
- Fatigue
- Lightheadedness
- Chest pain
- Syncope
Note: patients can be asymptomatic or describe that their heart is beating very fast or their heart "skips a beat"

1. Sinus Bradycardia
Sinus rhythm with a heart rate < 50 BPM
Treatment
- Only necessary if symptomatic
- Discontinue medications that cause bradycardia
- Administer atropine 0.5-1 mg IV, repeated every 3-4 minutes up to 3 mg total
**Refer to the full PowerPoint for treatment options due to overdosing on a myocardial suppressive medication
2. Sinus Tachycardia
Sinus rhythm with a heart rate > 100 BPM
Treatment
- Only treat when there is an unknown reason for tachycardia for a long time and at rest
- Beta-blockers
- Nondihydropyridine calcium channel blockers (Non-DHP CCBs)
3. Atrial Flutter
A short circuit going around the right atrium causes the atria to pump very rapidly. The upper chambers can contract up to 250-350 times per minute
There is an increased risk of stroke, heart failure, and additional heart rhythm problems
Treatment
- Slow the HR
- Rhythm control with cardioversion (medication/ablation)
- Prevent clots and stroke
4. Atrial Fibrillation (A-Fib)
Most common arrhythmia encountered in clinical practice!
The SA node is no longer controlling the heartbeat and there are multiple pulses sent from the atria to ventricles, but the AV node only contracts once.
Complications include stroke/thromboembolism, heart failure, and an increased risk of hospitalization and mortality
Types of A-Fib
- Paroxysmal - A-Fib that terminates spontaneously or with intervention within 7 days of onset
- Persistent - continuous A-Fib for > 7 days
- Long-standing persistent - Continuous A-Fib for > 12 months
- Permanent - Term used when the patient and clinician make a joint decision to stop further attempts to restore and/or maintain sinus rhythm
- Non-valvular - AF not involve any mitral stenosis or mechanical heart valves
Treatment
- First, determine if this is an emergency or not. An emergent presentation would be if the patient is in rapid ventricular response or is hemodynamically unstable
- Emergent cases
- Consider direct current cardioversion (DCC)
- **More on DCC in the full PowerPoint
- Start anticoagulation immediately and continue for at least 4 weeks
- Consider direct current cardioversion (DCC)
- If the patient presenting is a non-emergent case we need to think of two things:
- Rate vs Rhythm Control
- Anticoagulation
Rate vs Rhythm Control in A-Fib
Rate Control
- Use medications to slow conduction through the AV node
- Prefer when
- Asymptomatic
- Elderly
- Newly detected AF
- Medications
- Beta blockers
- Non-DHP CCBs (NOTE: contraindicated if LVEF </= 40%)
- Digoxin
- Amiodarone
Rhythm Control
- Anti-arrhythmic drug therapy and/or catheter ablation
- Prefer when
- Symptomatic
- Has heart failure
- Younger
- Failed rate control
- Medications (from Vaughn Williams Classification)
- Class I-A
- Class I-C
- Class III
- **Refer to full PowerPoint for VW Classification table and medications
Anticoagulation for A-Fib
Based on CHA2DS2-VASc score
Recommendation:
- Start oral anticoagulation if:
- CHA2DS2-VASc ≥ 2 (males)
- CHA2DS2-VASc ≥ 3 (females)
- Agents
- DOACs (first-line for most patients)
- Warfarin (goal INR 2-3)
**Refer to full PowerPoint for a breakdown of CHA2DS2-VASc
5. Paroxysmal Supraventricular Tachycardia (PSVT)
AV nodal reentrant tachycardia (AVNRT)
- The current reenters in the AV node and rapidly circles. This results in a fast heartbeat in both atria and both ventricles
- This is not life-threatening
- No need to treat if asymptomatic
Wolff-Parkinson-White Syndrome (WPW)
- When an extra muscle fiber connects the upper and lower chambers of the heart –> AVRT
- Catheter ablation is recommended
- With A-Fib or AVNRT, use ibutilide or procainamide
Treatment
- Regular PSVT/SVT
- BB or non-DHP CCBs
- Adenosine 6 mg IV push
- If the patient is unstable –> shock them
- SVT caused by AVNRT
- Asymptomatic –> no need to treat
- Symptomatic
- Catheter ablation if medications are ineffective
- No HFrEF
- BB/Non-DHP CCBs
- Flecainide/Propafenone
- HFrEF
- Amiodarone/digoxin/dofetilide/sotalol
6. Ventricular Tachycardia (V-Tach)
First determine if the patient has a pulse or not
- If without a pulse = this is a medical emergency!! Initiate ACLS (advanced cardiovascular life support)
V-Tach is defined as 3 or more consecutive ventricular complexes at a rate > 100 BPM
Types of V-Tach
- Non-sustained - 3 beats or more and terminates spontaneously
- Sustained - >30 seconds or requiring termination in < 30 seconds due to hemodynamic instability
- Monomorphic - Stable, single QRS with each beat
- Polymorphic - Changing/multiple QRS with each beat
Torsades de Pointes (TdP)
- A polymorphic ventricular tachycardia
- Due to prolongation of QT interval
- Potential causes
- Congenital long QT syndromes
- MI/heart failure
- Medications
Treatment
- If the patient is unstable, shock first
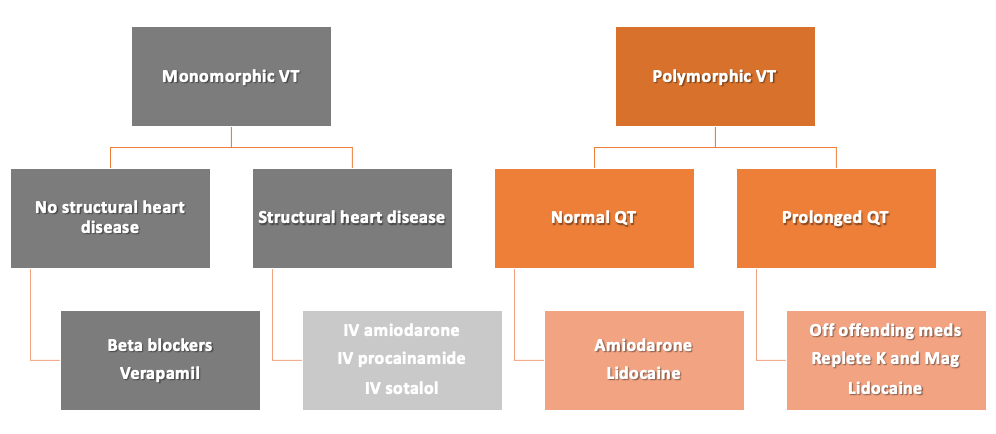
- **Refer to the full PowerPoint for treatment of hemodynamically stable V-Tach and implantable cardioverter defibrillator (ICD) placement recommendations
7. Ventricular fibrillation (V-Fib)
Untreated V-Tach can degenerate into V-Fib, which is a medical emergency
Hemodynamic collapse, syncope, cardiac arrest
Treatment
- Initiate Advance Cardiac Life Support (ACLS)
The full PowerPoint from Dr. Liang contains extra details on each arrhythmia such as:
- Causes for each type of arrhythmia
- Culprit medications that can induce each arrhythmia
- Mechanism of action of the medications used to treatment arrhythmia
- EKG examples of each arrhythmia (also shown below)
References
- Noel ZR and Tisdale JE. Arrhythmias. ACCP/ASHP Cardiology Pharmacy Preparatory Review and Recertification Course
- Al-Khatib SM, Stevenson WG, Ackerman MJ, et al.2017 AHA/ACC/HRS Guideline for Management of Patients With Ventricular Arrhythmias and the Prevention of Sudden Cardiac Death: A Report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines and the Heart Rhythm Society. J Am Coll Cardiol. 2018 Oct 2;72(14):e91-e220.
- January CT, Wann LS, Calkins H, et al. 2019 AHA/ACC/HRS Focused Update of the 2014 AHA/ACC/HRS Guideline for the Management of Patients With Atrial Fibrillation: A Report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines and the Heart Rhythm Society. J Am Coll Cardiol. 2019 Jul 9;74(1):104-132.
- Algorithms. AHA CPR & First Aid Emergency Cardiovascular Care. https://cpr.heart.org/en/resuscitation-science/cpr-and-ecc-guidelines/algorithms#adult (accessed Aug 22, 2023)