Emergency Medicine Review: TBI Management
Overview of key TBI pharmacotherapy: RSI, sedation, hemodynamics, hyperosmolar therapy, seizure & anticoagulant management for acute care. Robbins 2025 AJEM article discussed.
I was searching for new articles to cover for a journal club post. I came across this narrative review of Traumatic Brain Injury in the American Journal of Emergency Medicine, and it took me back to my residency training. After reading the article as a refresher, I thought, "This would be a great article to do a high-level overview on for RxTeach!"
So, instead of a traditional journal club, today's post will be akin to a topic discussion: a "too long, didn't read" style. The information we will cover today is important for acute settings such as an emergency department or ICU where "time is tissue", and weight-based dosing for certain agents is handy to have drilled into your memory bank.
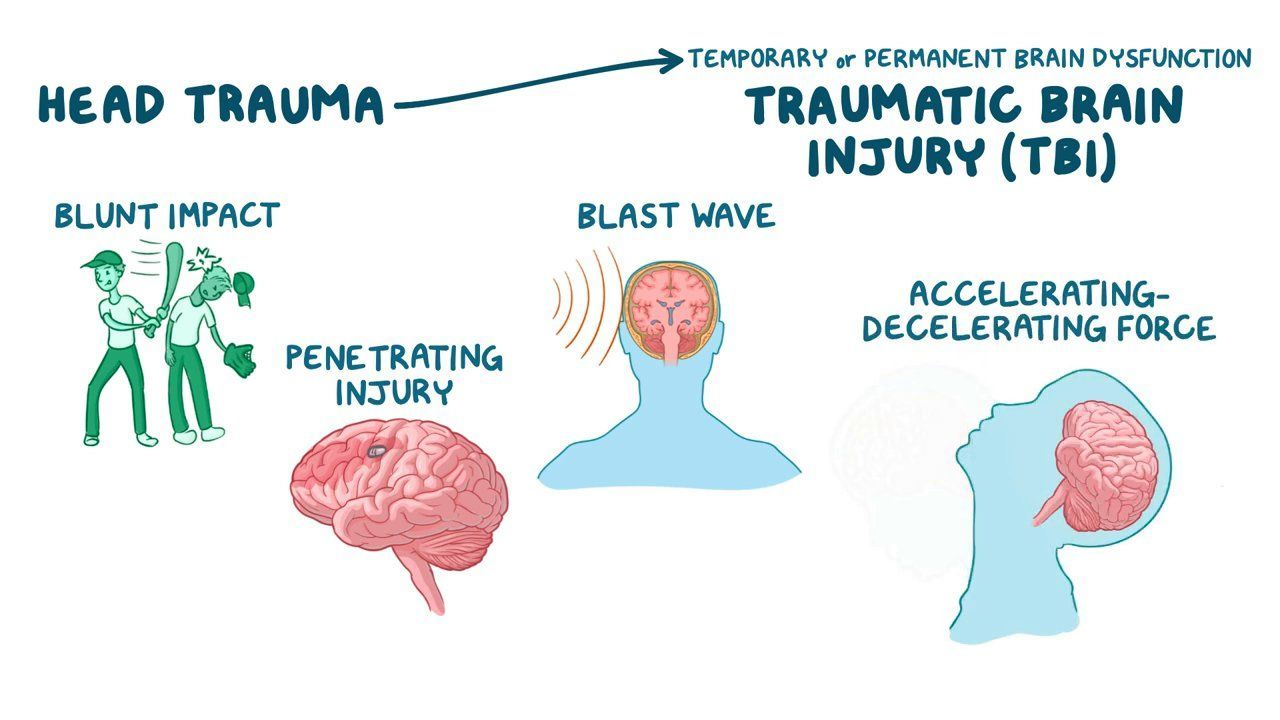
Introduction
A traumatic brain injury (TBI) is caused by a violent blow/jolt to the head or by an object that penetrates brain tissue (Mayo Clinic). TBI is a significant global health concern and if you have worked in a trauma center or acute care facility, you may be familiar with the urgency of care required to care for these patients.
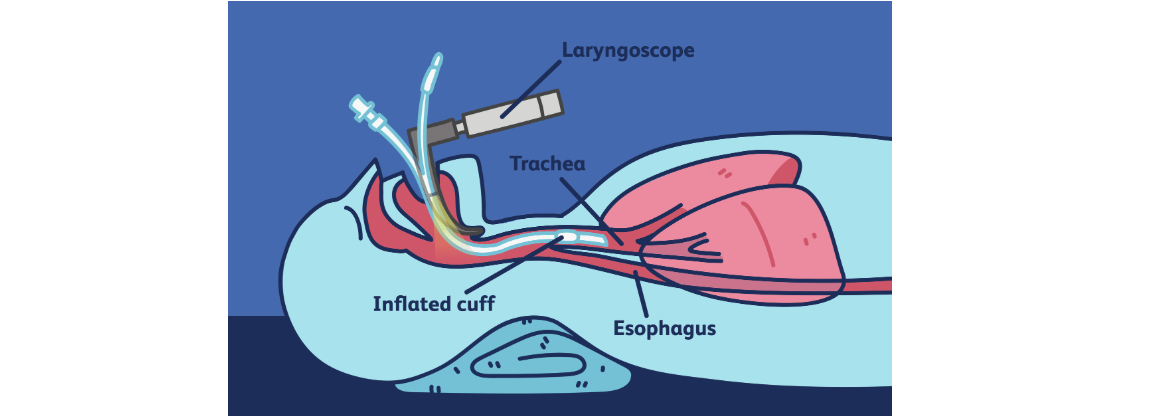
Upon arrival to the emergency department (ED), considering the patient's ABCs are of utmost concern.
- A - airway
- B - Breathing
- C - circulation
Rapid Sequence Intubation (RSI) and Post-Intubation Management
Goal: Secure the airway while minimizing increases in intracranial pressure (ICP), prevent hypotension, and allow for neurological assessment.
Medications in RSI are for pre-medication, induction, & paralyzation.
- Body weight is often used for dosing in these emergent situations
- Pre-medications - purpose is to blunt sympathetic stimulation to minimize increases in ICP
- Lidocaine - limited evidence to blunt sympathetic stimulation, can cause hypotension and arrhythmias. Not recommended.
- Fentanyl - literature supports ability to attenuate increases in ICP. Recommended dosing in RSI is 2-3 mcg/kg IV.
- Induction - purpose is to minimize hemodynamic effects and decline in mean arterial pressure (MAP) and subsequent decrease in cerebral perfusion pressure (CPP).
- Etomidate - minimal impact on hemodynamics, cerebral protective properties. Recommended dosing in RSI 0.3 mg/kg IV.
- Ketamine - analgesic, dissociative, and sympathomimetic properties. Recommended dosing in RSI 1-2 mg/kg IV once over 1 minute. If patient in shock, reduce dose to 0.5-1 mg/kg.
- Propofol - rapid onset and offset of action, commonly used in post-intubation sedation. Recommended dosing in RSI 1.5-2 mg/kg IV once. An additional continuous IV infusion may be required for post-intubation sedation.
- No clear difference between all three agents in hemodynamic effects.
- Paralytic agents - purpose is to paralyze the patient during intubation and allow for neurological assessment after intubation
- Succinylcholine (depolarizing) - short duration of action (5-10 min) for timely neurological assessments, low quality of evidence to suggest it can increase ICP. Recommended dosing in RSI is 1-1.5 mg/kg IV.
- Rocuronium and Vecuronium (non-depolarizing) - 20-80 min duration which requires timely initiation of sedation to prevent the patient from waking in a paralyzed state. Both recommended, although vecuronium is typically used only when succinylcholine or rocuronium are unavailable. Rocuronium dosing in RSI is 1-1.2 mg/kg IV once. Vecuronium dosing in RSI is 0.1-0.2 mg/kg IV once.
- Sugammadex - a reversal agent for rocuronium and vecuronium - can tackle the primary disadvantages of these agents. Dosed as 2-4 mg/kg IV.
- No preference for a single paralytic agent in RSI due to lack of high-quality trials.
Medications in Post-Intubation Management are for sedation & pain.
- Sedation agents - purpose is to minimize the chance of the patient waking up in a paralyzed state and self-extubating
- Propofol - continuous infusion agent, short half-life, can achieve deep sedation, can decrease ICP, anti-epileptic properties. First-line option.
- Midazolam - longer duration of activity for amnesia, can achieve deep sedation at higher doses, anti-epileptic properties.
- Dexmedetomidine - amnestic effects but not able to achieve deep sedation or anti-epileptic properties. Not recommended in patients who may still be pharmacologically paralyzed.
- Analgesic agents
- IV push opioids such as hydromorphone, fentanyl, and morphine.
- Continuous infusions of opioids may be required and beneficial during initial and optimization stage of RSI.
Hemodynamic Management
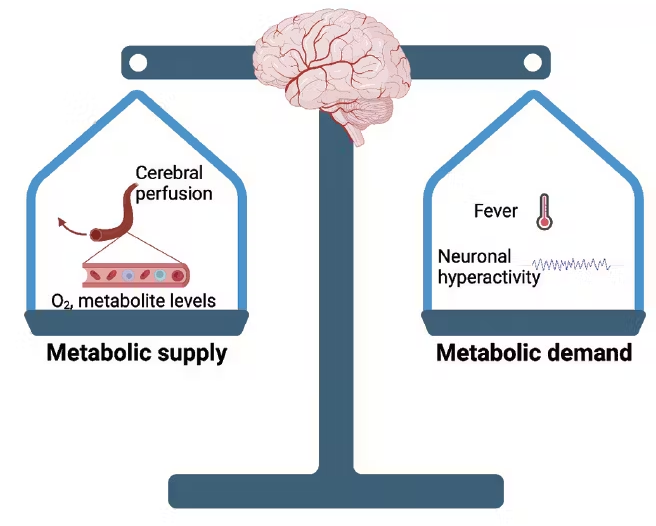
Goal: maintain cerebral perfusion pressure (CPP) while preventing hematoma expansion.
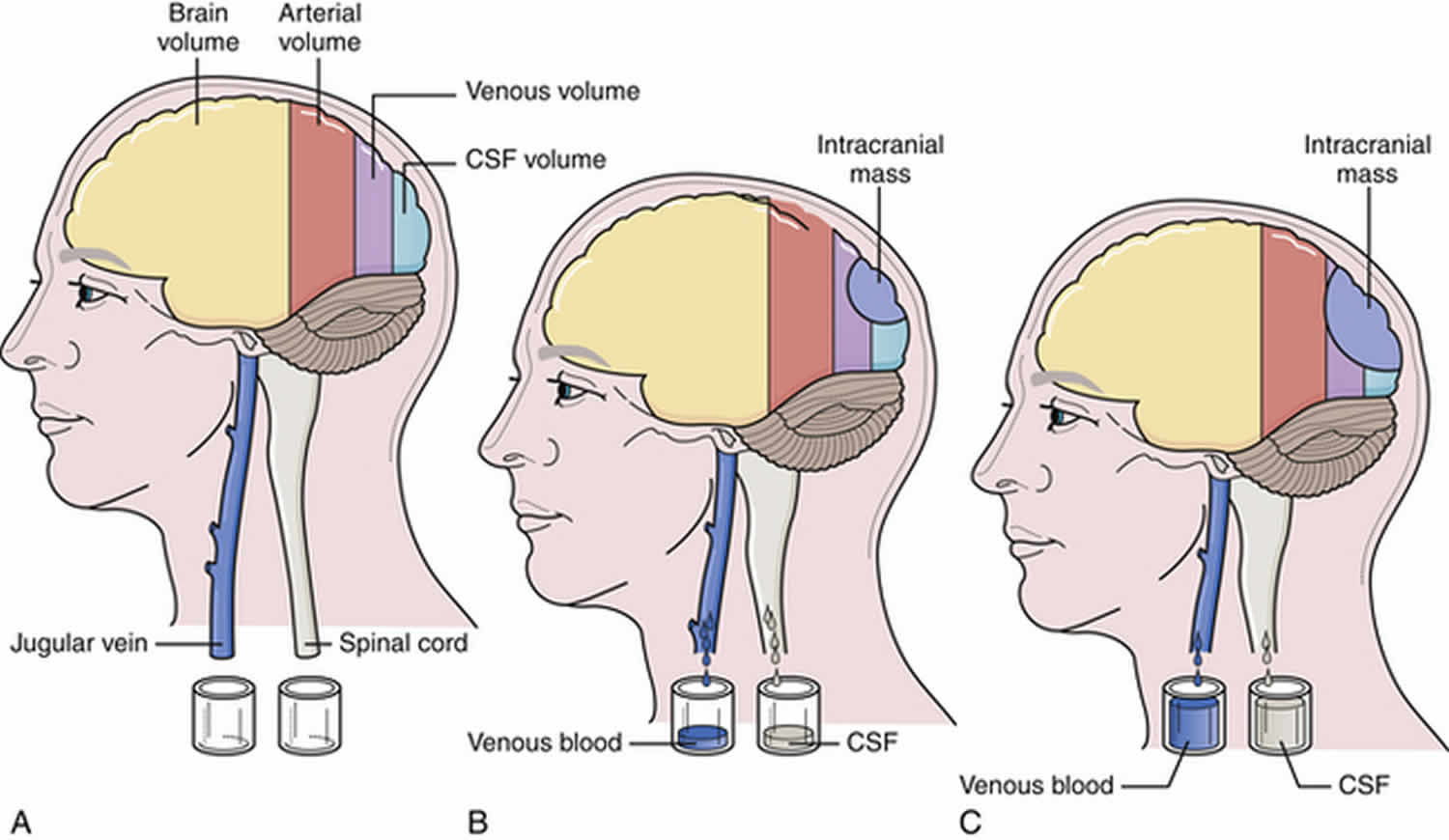
In normal physiology, a drop in systolic blood pressure (SBP) leads to vasodilation to maintain adequate cerebral perfusion and increased cerebral blood volume which increases ICP. In TBI, the normal physiology is not intact, and cerebral perfusion is dependent on SBP to prevent cerebral ischemia.
Recommendation: maintain SBP at or above 100-110 mmHg (depending on the age of the patient)
Hypotensive patients and maintaining SBP
- Fluid resuscitation - helps to restore or maintain intravascular volume to improve cerebral blood flow, limit cerebral hypoxia and ischemia, and prevent elevations in ICP.
- Pre-hospital/acute setting
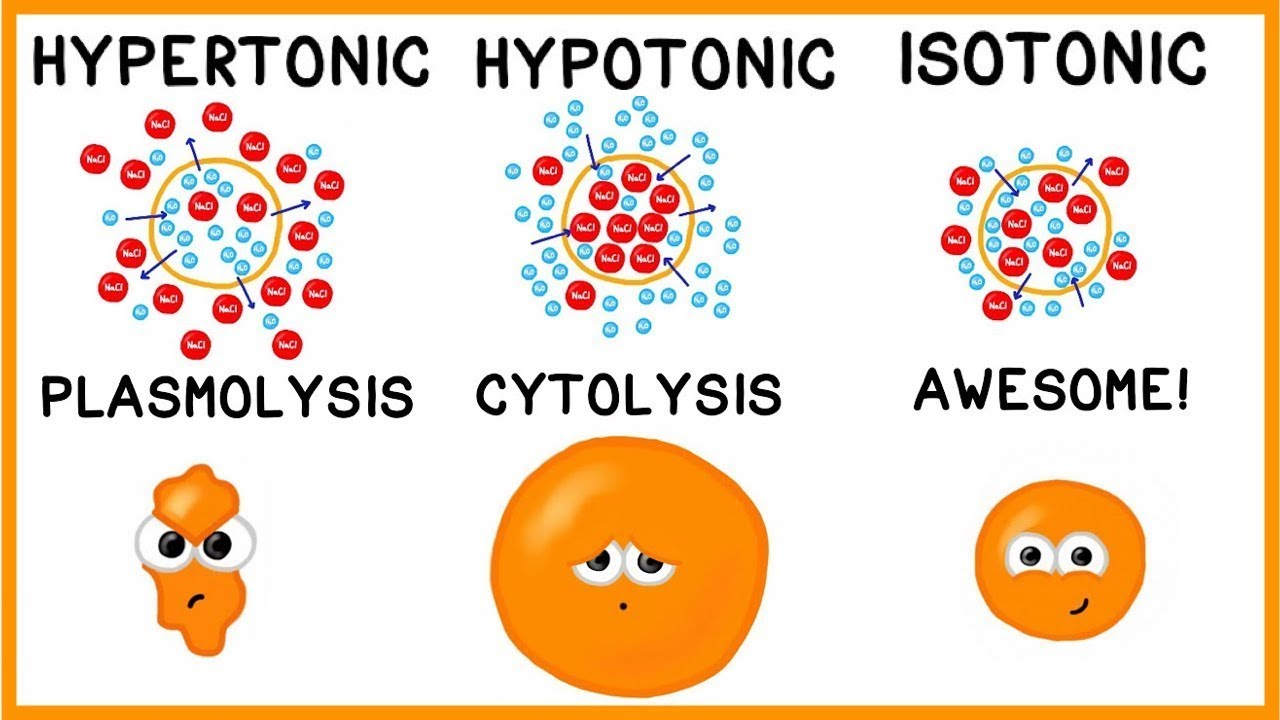
- Hypotonic fluids are LESS desirable due to the potential increase in cerebral edema.
- Pre-hospital/acute setting
- However, several studies and meta-analyses have found no difference between hypotonic, isotonic, or hypertonic fluids.
- IV Fluids Guide for identifying hypo/iso/hypertonic solutions.
- Guideline recommendations: start maintenance fluids at 30 mL/kg/day to maintain euvolemia. Isotonic fluids are generally preferred.
- Vasoactive agents - used if fluid resuscitation is unable to achieve euvolemia.
- Norepinephrine - 0.05-0.15 mcg/kg/min continuous IV infusion, titrated based on MAP.
- Phenylephrine - 0.5-2 mcg/kg/min continuous IV infusion, titrated based on MAP.
- Vasopressin - 0.03 units/min continuous IV infusion, used as an add-on to other vasoactive agents.
- No single agent is preferred.
Hypertensive patients (SBP ≥140 mmHg)
Higher SBP in TBI patients is due to the activation of catecholamine release pathways from brain injury which elevated ICP.
Mortality rate = 21% when SBP <120 mmHg
Mortality rate = 9% when SBP 120-140 mmHg
Mortality rate = 19% when SBP ≥140 mmHg
No consensus for HTN treatment exists in the TBI population.
- Anti-hypertensive agents
- Nicardipine via continuous infusion - rapid onset and short duration of action. Less variability and need for rescue therapy compared to labetalol and hydralazine. Recommended dosing starts at 5 mg/hr and titrated by 2.5 mg/hr based on SBP control.
- Clevidipine - 1-2 mg/hr continuous IV infusion, titrated based on SBP. Preferred alternative if nicardipine is unavailable.
- Nitroprusside - 0.25-0.5 mcg/kg/min continuous IV infusion, titrated based on SBP. Use for the shortest duration possible to avoid toxicity. This agent is used when other preferred agents are unavailable.
Hyperosmolar Therapies
TBI can lead to cerebral edema which contributes to increases in ICP. This is thought to be due to multiple processes, both vasogenic and cytotoxic edema. Hyperosmolar therapies can mobilize fluid out of the skull via intravascular osmolality gradients. Both agents below are relatively impermeable to an intact blood-brain barrier; that is how a gradient is formed to draw fluid out of the cerebral space.
- Hyperosmolar agents
- Note: quality of evidence to support the use of hyperosmolar agents in TBI remains low. ICP reductions have been shown, but there is no definitive data on mortality reduction or neurologic function improvement.
- Hypertonic saline (HTS; >0.9% saline) - up to 23.4% has demonstrated safety and efficacy via intermittent IV boluses via peripheral or central access. HTS is recommended over mannitol per the NCS potentially due to a more rapid onset of action and durable reduction in ICP. Recommended dosing for 3% HTS is 2-5 mL/kg over 5-20 minutes. Recommended dosing for 23.4% HTS is 0.6-0.6 mL/kg (max of 30 mL) over 10-20 minutes.
- Mannitol 20% - clearance can be reduced in patients with renal disease. Mannitol may worsen hypovolemia as it has a diuretic effect. Recommended dosing is 0.25-1 g/kg over 5-15 minutes.
- If either agent is used, monitor for IV extravasation, elevations in sodium and osmolality, and electrolyte imbalances.
- Upper limit of serum sodium = 155-160 mEq/L
- Upper limit of serum chloride = 110-115 mEq/L
Management of Coagulopathy
Coagulopathy from trauma is multifactorial, and one proposed mechanism to aid in the management of coagulopathy is to target fibrinolysis.
- Antifibrinolytic agents
- Tranexamic acid - studies demonstrate a mortality benefit with tranexamic acid administration within 3 hours of injury. Data in isolated head injuries are limited. the CRASH 2 and 3 studies looked at 1 g of tranexamic acid IV over 10 minutes followed by 1 g over 8 hours. These studies showed no difference in head injury death within 28 days, but there was a reduction in this outcome in the subset of patients with mild to moderate head injury who received tranexamic acid. Routine administration of tranexamic acid in TBI is not fully supported by current evidence.
If the patient presents with a TBI and concurrent anticoagulation therapy (such as warfarin or a DOAC), assessment for appropriateness of reversal of the anticoagulant is warranted. Reversal can lead to thrombosis, so the risks versus benefits must be weighed.
- Causes hemodynamic instability,
- Decreases hemblogin >2 g/dL,
- Requires ≥2 units of red blood cells,
- Occurs in a critical site such as the brain, or
- The patient requires emergency surgery
- Anticoagulant reversal agents
- Prothrombin complex concentrate (PCC) 3 or 4 (preferably 4) - for reversal of warfarin and also used in DOAC reversal, especially if andexanet alfa is unavailable (which is common). Dosing based on INR and weight. Some institutions may have fixed-dose protocols.
- NOTE: Contraindicated if patients have a heparin allergy. PCC contains heparin.
- Phytonadione (Vitamin K) - for reversal of warfarin. Use in conjunction with PCC. IV route preferred in acute reversal situations.
- Fresh frozen plasma (FFP) - alternative if PCC is not available. Dosed at 0-15 mL/kg. Less effective at reversing warfarin and can exacerbate cerebral edema.
- Andexanet alfa - for reversal of DOACs (apixaban, rivaroxaban, etc).
- Protamine - for reversal of heparin if given in the previous 2-3 hours or enoxaparin if previous dose was given in the last 12 hours.
- Idarucizumab - for reversal of dabigatran. Use FFP if unavailable.
- Prothrombin complex concentrate (PCC) 3 or 4 (preferably 4) - for reversal of warfarin and also used in DOAC reversal, especially if andexanet alfa is unavailable (which is common). Dosing based on INR and weight. Some institutions may have fixed-dose protocols.
Seizure Prophylaxis
Rates are post-traumatic seizures are as high as 12%, and guidelines recommend antiseizure prophylaxis in hospitalized patients with moderate-severe TBI for up to 7 days.
- Antiseizure agents
- Phenytoin - largest body of evidence, but does have risk of hypotension, cardiac arrhythmias, drug-drug interactions, and requires drug monitoring. Recommended dosing for prophylaxis in TBI is 100 mg q8h or 5 mg/kg/day divided every 8 hours IV or PO for 7 days.
- Levetiracetam - minimal drug-drug interactions, side effects and no drug monitoring required. Preferred over phenytoin in most settings. Recommended dosing for prophylaxis in TBI is 1 g q12h IV or PO for 7 days.
- Valproate - associated with no benefit and higher mortality. Not recommended.
- Carbamazepine - data to support reduction in seizure activity, but has several drug-drug interactions and is not available in IV formulations. Not recommended.
- Phenobarbital - lack of data to support use and also had numerous drug-drug interactions. Not recommended.
Antibiotic Prophylaxis
Due to the nature of TBIs, the skull is typically fractured and patients are at risk for infection.
- Antibiotic agents
- Vancomycin - gram-positive bacteria coverage. Dosed with a 25 mg/kg IV infusion loading dose and 15 mg/kg IV infusion maintenance doses. Continue to adjust based on troughs (goal 15-20 mcg/mL) or AUC (400-600).
- Anti-pseudomonal agent (cefepime, ceftazidime, meropenem, aztreonam, ciprofloxacin) - beta-lactam preferred unless patient is allergic. Provides gram-negative bacteria coverage.
- Multiple meta-analyses conclude there is no supporting evidence to recommend prophylactic antibiotics in TBI for decreasing the rate of meningitis.
- However, patients with cerebral spinal fluid leak are at an increased risk for meningitis, and data suggest this subgroup of patients may benefit from preventative antibiotic therapy.
Reference:
- Blake Robbins, Lars Almassalkhi, Regan Baum, et al. Pharmacotherapy adjuncts for traumatic brain injury: A narrative review of evidence and considerations in the emergency department. AJEM 2025;89:78-84. https://www.sciencedirect.com/science/article/abs/pii/S0735675724006879
- Lexicomp Online 2025
*Information presented on RxTeach does not represent the opinion of any specific company, organization, or team other than the authors themselves. No patient-provider relationship is created.

