Penicillin Panic: Are You Really Allergic?
Many penicillin allergy labels are inaccurate, creating barriers to care. Learn how tools like PEN-FAST help de-label and improve treatment.
You experience it all the time. A patient needs treatment for their infection, and you proceed to order penicillin only to be hit with a huge warning sign alerting you of a penicillin allergy. Whether you find that yourself as the clinician ordering penicillin or the patient who has the documented allergy, it's evident to everyone just how much of a barrier and inconvenience to optimal and efficient care this situation can be.
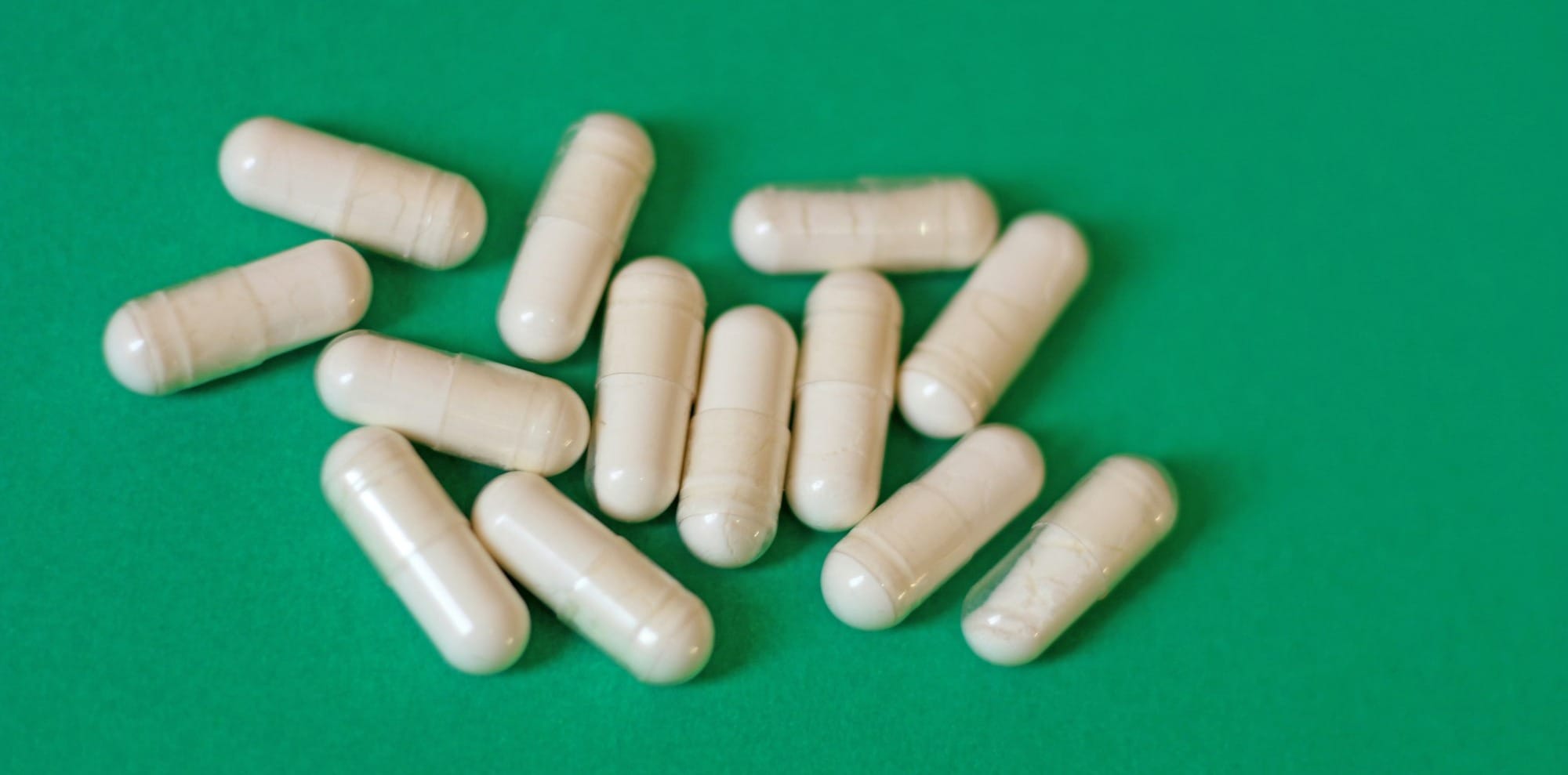
Worldwide, about 9.4% of people report having a penicillin (PCN) allergy1. To put this into perspective, there is about 8 billion people worldwide. 9.4% of 8 billion is about 750 million people who say they have a PCN allergy. That is more people than the entire population of Europe (currently around 745 million as of April 2025)! This statistic also holds relatively true within the United States as about 10% of people here report having a PCN allergy per the CDC2. In reality though, less than 1% of people have a true PCN allergy.
Most of the PCN allergies reported by adults come from a mild reaction or event that occurred when they were a child3,4. Sometimes, people may remember the specific incidence and reaction that occurred. Other times it may be that a family member has mentioned there was an allergic reaction many years ago and strictly forbids the use of any PCN. Regardless of which scenario you or your patient is in, it's important to recognize the impact that reporting a PCN allergy can have. Distinguishing a true allergy is key when it comes to providing patients with appropriate therapy in a timely manner.
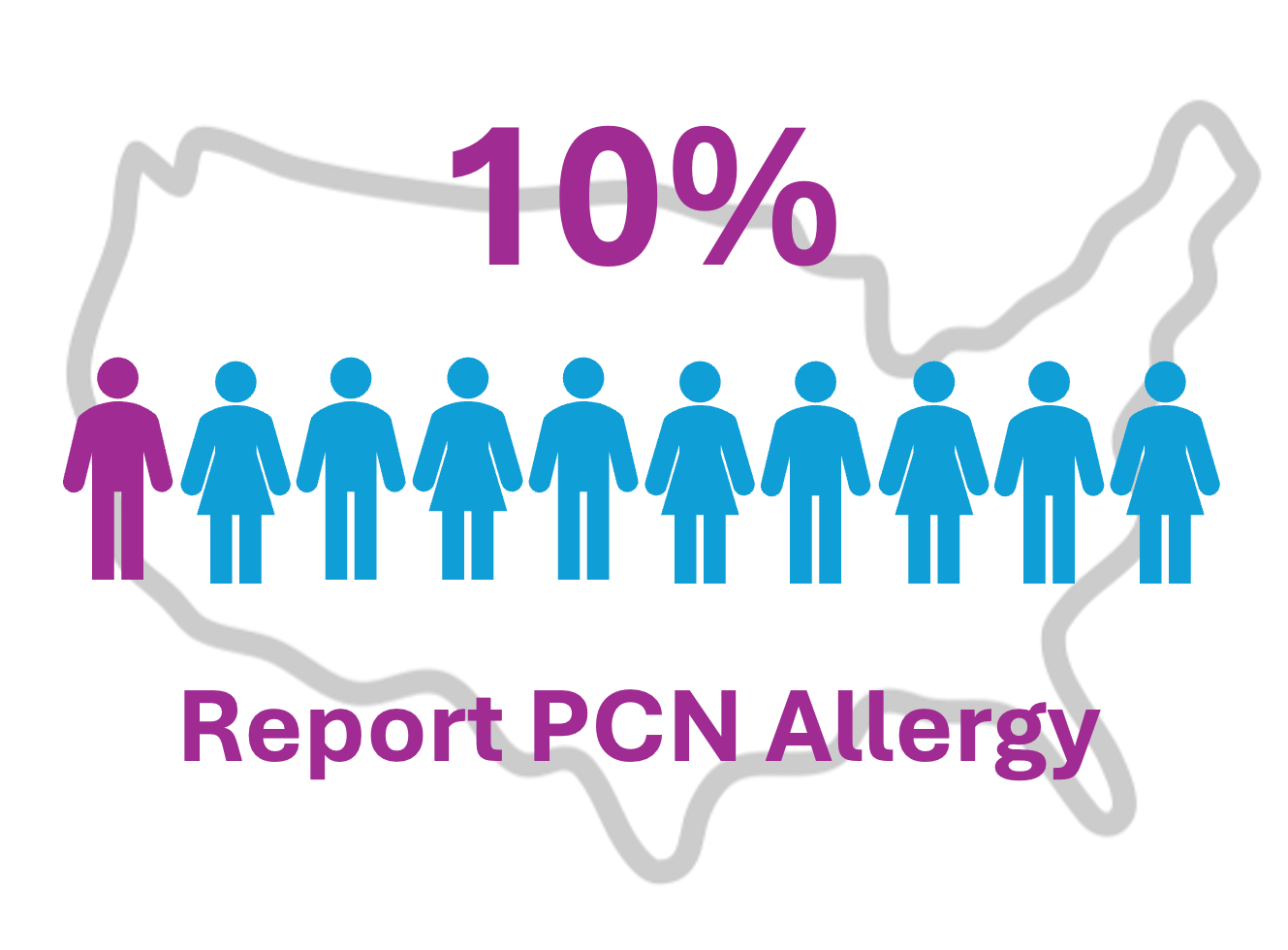
So, what do I mean when I say "true" PCN allergy? You might think that having a drug allergy is as simple as having a bad reaction or side effect to a drug is it not? Unfortunately, it's not that simple. There are four main types of allergic reactions (hypersensitivities) mediated through different mechanisms and induced by various drugs. Furthermore, these four hypersensitivities can be categorized as "immediate" or "delayed". I won't go through drug hypersensitivities today (keep a lookout for a future article!), but as a quick review, see the graphic below.
When we refer to "true" PCN allergies, these are ones that generally fall under Type I: IgE-mediated anaphylaxis reactions. PCN technically has a chance to induce all four hypersensitivity types, but the most common are I and IV5. This is why it's so important to distinguish between a true PCN allergy vs. a "pseudo-allergy" or mild reaction. When it comes to treating infections, it's necessary to weigh the risk vs. benefits. For true PCN allergies, the risk far outweighs the benefits as anaphylaxis may lead to death. However, for those who have a milder reaction or a pseudo-allergy to PCN may have a greater benefit depending on the type of infection that's being treated.
So, how do we know if a patient has a true PCN allergy? The traditional method of testing for allergy is a PCN skin test6. It involves administering a small amount of PCN to the skin with a tiny needle. A positive reaction to a test will cause a red, itchy, raised bump. While the PCN skin test can be and still is an excellent method to use today, it still comes with several limitations. The skin test has a low sensitivity and high specificity7. This means that while a positive test result is more likely to indicate a true penicillin allergy, a negative result doesn't rule it out entirely. What's more is that the test is designed to generally only detect immediate-type hypersensitivities. It will not detect Type IV: Cell-mediated reactions. Finally, it does involve using a small needle to puncture the skin which some individuals may dislike.
These limitations can pose a potential barrier to effectively using PCN. More recently a newer method called the PEN-FAST tool was created. The PEN-FAST tool was first developed and tested by Dr. Jason Trubiano and colleagues in 2020. It enables point-of-care risk assessment of patient-reported PCN allergies8. This quick tool can be used by any healthcare worker and is extremely helpful in emergency department settings where time efficiency is really important. It doesn't require any use of needles as all that is required is to just speak and ask the patient a few questions. Here's what PEN-FAST entails:
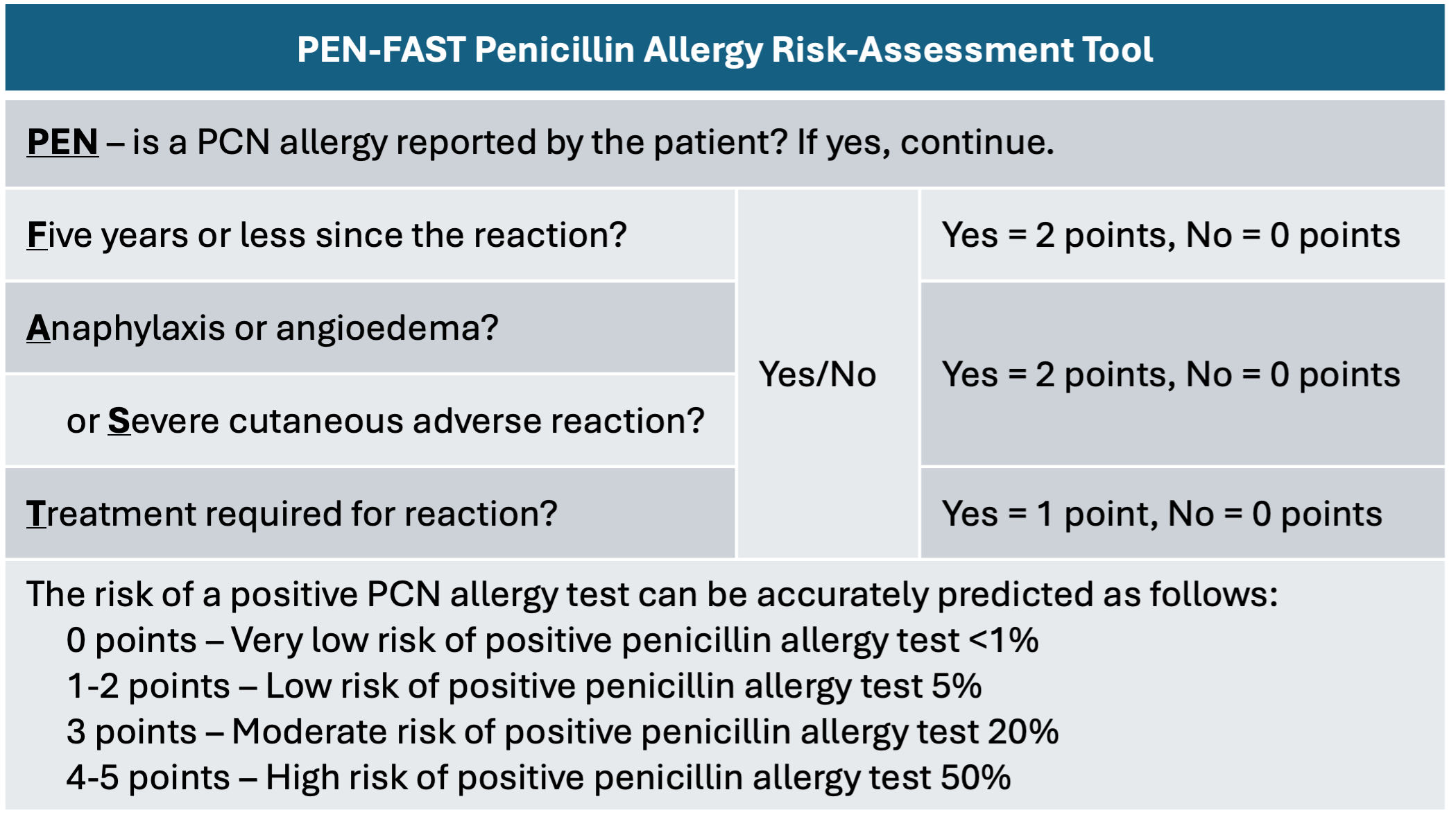
There are five very simple and straightforward questions to ask patients. First, does the patient report a PCN allergy in the first place? If yes, continue with the remaining questions. Second, did the reported PCN allergy occur within the last five years? If yes, 2 points. Third and fourth, did the allergy include anaphylaxis, angioedema (severe swelling), and/or a severe skin reaction? If yes, 2 points. Finally, was any treatment given to help treat the reaction (such as antihistamines or another drug)? If yes, 1 point. In total a patient may score a maximum of 5 points, indicating that they are at higher risk of a positive PCN allergy test and thus may be truly allergic. We should avoid initiating PCN (or any other related beta-lactam antibiotics) in these patients.
The utility and effectiveness of the PEN-FAST tool has been studied in a variety of settings, including the emergency department. In a recent study by Tran and colleagues, they aimed to determine the safety and efficacy of their facility's implementation of pharmacist utilization of the PEN-FAST screening tool to assess purported penicillin allergies and re-challenge low to moderate risk patients in the ED9. In their prospective, observational study including 100 patients they found that administration of beta-lactam antibiotics to ED patients with previously reported penicillin allergies and a PEN-FAST score less than 3 did not result in any immune-mediated reactions. This meant that the PEN-FAST decision tool was able to safely identify and risk-stratify eligible patients for beta-lactam re-challenge in the ED.
Probably one of the most robust pieces of evidence for the use of PEN-FAST comes from the PALACE randomized clinical trial performed by Copaescu and colleagues10. The study compared whether low-risk PCN allergy labels (scored using PEN-FAST) needed to have the traditional skin testing before taking an amoxicillin test dose, vs. taking a test dose without skin testing. The results were non-inferior and found that an estimated 1 out of 200 patients with low-risk allergy label had a rash, regardless of whether skin testing was performed. This meant that skin testing was really not needed at all in order to "de-label" a low-risk PCN allergy from a patient's profile.

Being able to de-label a PCN allergy from a patient's profile can provide immense benefits for treatment regimens. For one, the patient would be able to take PCN for any treatment that requires it. The patient would also be able to take a variety of other antibiotics including beta-lactams, which have potential cross-reactivity with PCN allergies. This opens up huge avenues for antibiotic options as beta-lactams are some of the most common antibiotics used in infection treatment and goes together with effective antibiotic stewardship.
Speaking of cross-reactivity, I'd like to bring up another excellent method for allergy antibiotic stewardship for implementation. It involves the medicinal chemistry of beta-lactam antibiotics. The primary reason that beta-lactams have different spectra of activity, adverse effects, pharmacokinetics, etc. is because of their unique side chains. All beta-lactams contain the common beta-lactam ring. Their differences come in the form of unique R1 and/or R2 side chains. Depending on which side chains each antibiotic has in common, you may or may not have to worry about a PCN allergy at all. See this amazing chart below from Northwestern Memorial Antimicrobial and Diagnostic Stewardship program:
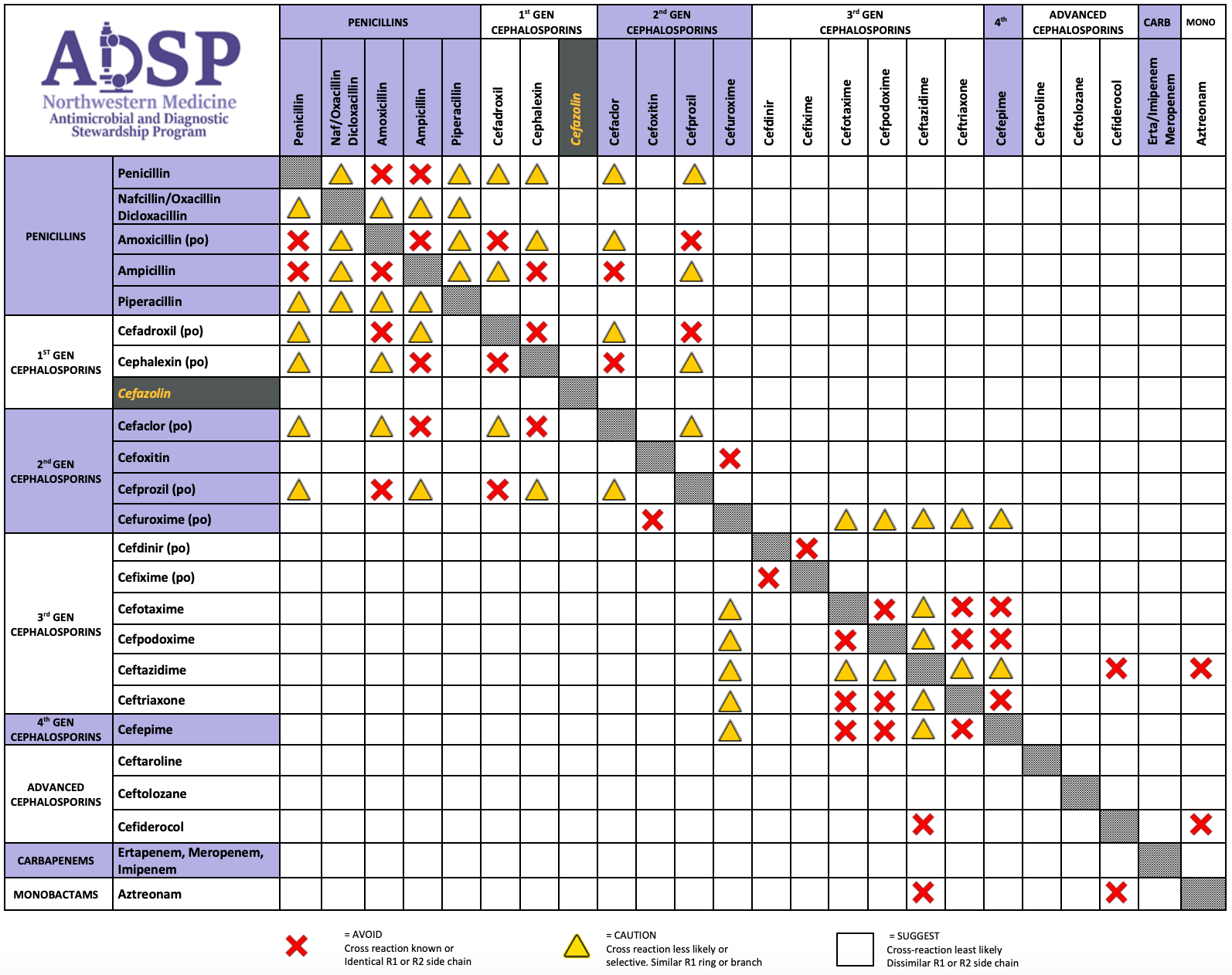
A red "X" means that the PCN or beta-lactam antibiotic shares an R1 or R2 side chain with the other referenced PCN or beta-lactam. For example, look at three boxes to the right from the top-left most grey box in the chart. There is a red X referring to the drug PCN (if looking from the left) and the drug amoxicillin (if looking from the top). This means that PCN and amoxicillin share an R1 or R2 side chain. Both PCN and amoxicillin should be avoided if the patient has a true PCN allergy label. Yellow triangles mean that the drug has a similar R1 or R2 side chain and so you should proceed with caution if you want to administer that specific antibiotic in a setting with a PCN allergy label.
Finally, any blank boxes mean that the antibiotic shares no R1 or R2 side chains with the other referenced drug. You are ok to proceed with administering that particular antibiotic if the patient is allergic to the other. Take for example the antibiotic cefazolin. Notice that the entire row (and column if looking from the top) of cefazolin is blank. This means cefazolin has a completely unique side chain from all other PCNs and beta-lactams. In the setting of any other PCN or beta-lactam allergy, cefazolin may be given if it is not listed as a specific allergy itself. Cefazolin has been found to be an extremely unique scenario, and may be given without prior testing in patients with a previous history of anaphylaxis to PCN.
About 10% of people both worldwide and within the United States report having a PCN allergy. But is this a true allergy? It's vital for both clinicians and patients to recognize that a reaction during childhood may not correlate directly to a complete contraindication to PCN and related antibiotics. It is imperative that healthcare professionals review with patients carefully the history of their reactions and other considerations, to determine whether that pesky PCN allergy label can finally be de-labeled.

References:
- Luintel A, Healy J, Blank M, et al. The global prevalence of reported penicillin allergy: A systematic review and meta-analysis. J Infect. 2025;90(2):106429. doi:10.1016/j.jinf.2025.106429
- Stone Jr. C. Antibiotic Stewardship when an Allergy Label is Present Improves Our Antibiotic Care and Treatment Outcomes. CDC. 2023; https://blogs.cdc.gov/safehealthcare/antibiotic-stewardship-and-allergy-labels/
- Trubiano JA, Adkinson NF, Phillips EJ. Penicillin Allergy Is Not Necessarily Forever. JAMA. 2017;318(1):82-83.
- Norton A, Konvinse K, Phillips E, Broyles A. Antibiotic Allergy in Pediatrics. Pediatrics. 2018;141(5).
- Patterson RA, Stankewicz HA. Penicillin Allergy. [Updated 2023 Jun 20]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2025 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK459320/
- https://www.mayoclinic.org/diseases-conditions/penicillin-allergy/diagnosis-treatment/drc-20376226
- Sousa-Pinto B, Tarrio I, Blumenthal KG, et al. Accuracy of penicillin allergy diagnostic tests: A systematic review and meta-analysis. J Allergy Clin Immunol. 2021;147(1):296-308. doi:10.1016/j.jaci.2020.04.058
- Trubiano JA, Vogrin S, Chua KYL, et al. Development and Validation of a Penicillin Allergy Clinical Decision Rule. JAMA Intern Med. 2020;180(5):745-752. doi:10.1001/jamainternmed.2020.0403
- Tran K, Lund J, Sealy C, Langley D, Kisgen J. PEN-FAST-ED: Utilizing the PEN-FAST decision tool to guide antibiotic prescribing in the emergency department. Am J Emerg Med. 2025;90:124-128. doi:10.1016/j.ajem.2025.01.039
- Copaescu AM, Vogrin S, James F, et al. Efficacy of a Clinical Decision Rule to Enable Direct Oral Challenge in Patients With Low-Risk Penicillin Allergy: The PALACE Randomized Clinical Trial. JAMA Intern Med. 2023;183(9):944-952. doi:10.1001/jamainternmed.2023.2986
*Information presented on RxTeach does not represent the opinion of any specific company, organization, or team other than the authors themselves. No patient-provider relationship is created.