Syphilis
Buckle up for a quick run down of one intricate disease, syphilis! Dr. White is here to introduce us to syphilis, the different stages, and how to treat the disease!

Author: Brett White, PharmD
Editor: Kristen Lindauer, PharmD, BCPS
Welcome back for another guest-lead topic discussion! Dr. Brett White, a current PGY1 resident at Sentara Norfolk General Hospital, recently presented a topic discussion on Syphilis during his infectious diseases rotation. Brett has a passion for infectious diseases, and is a ray of positive energy in the hospital. He is excited to share his introduction to Syphilis with you!
Dr. White's PDF handout will be available to paid subscribers only. You can find the links at the bottom of this article. If you are not a paid subscriber, but would like access to our bonus content, go to our homepage, click on the “Subscribe” button, and select the tier you would like to subscribe to for premium RxTeach content!
Let's dive into the topic!

Introduction
Treponema pallidum is a gram negative bacterium that causes syphilis. T. pallidum is a member of the phylum spirochaetota, which is generally referred to as "spirochetes." Syphilis is a sexually transmitted disease that effects the skin and mucous membranes of the external genitalia and mouth. The majority of syphilis cases are in men-who-have-sex-with-men (MSM). According to the CDC, MSM account for 36% of all primary and secondary syphilis cases in 2021. Case rates have increased in heterosexual men and women recently. Congenital syphilis also continues to be a concern in the US and occurs when a mother passes syphilis to her baby.
Transmission and Presentation
- Sexual contact with an infected partner
- Via direct contact with a syphilitic sore (aka a chancre)
- Chancres can develop around the penis, vagina, anus, rectum, lips, or mouth
- Congenital: likelihood of in-utero transmission correlates with mother’s stage of disease
After exposure and infection, symptoms begin (on average) in 21 days. The range of symptom onset has been documented between 10-90 days.
The symptoms will gradually develop and become more severe over time. We divide the severity of symptoms into "stages."
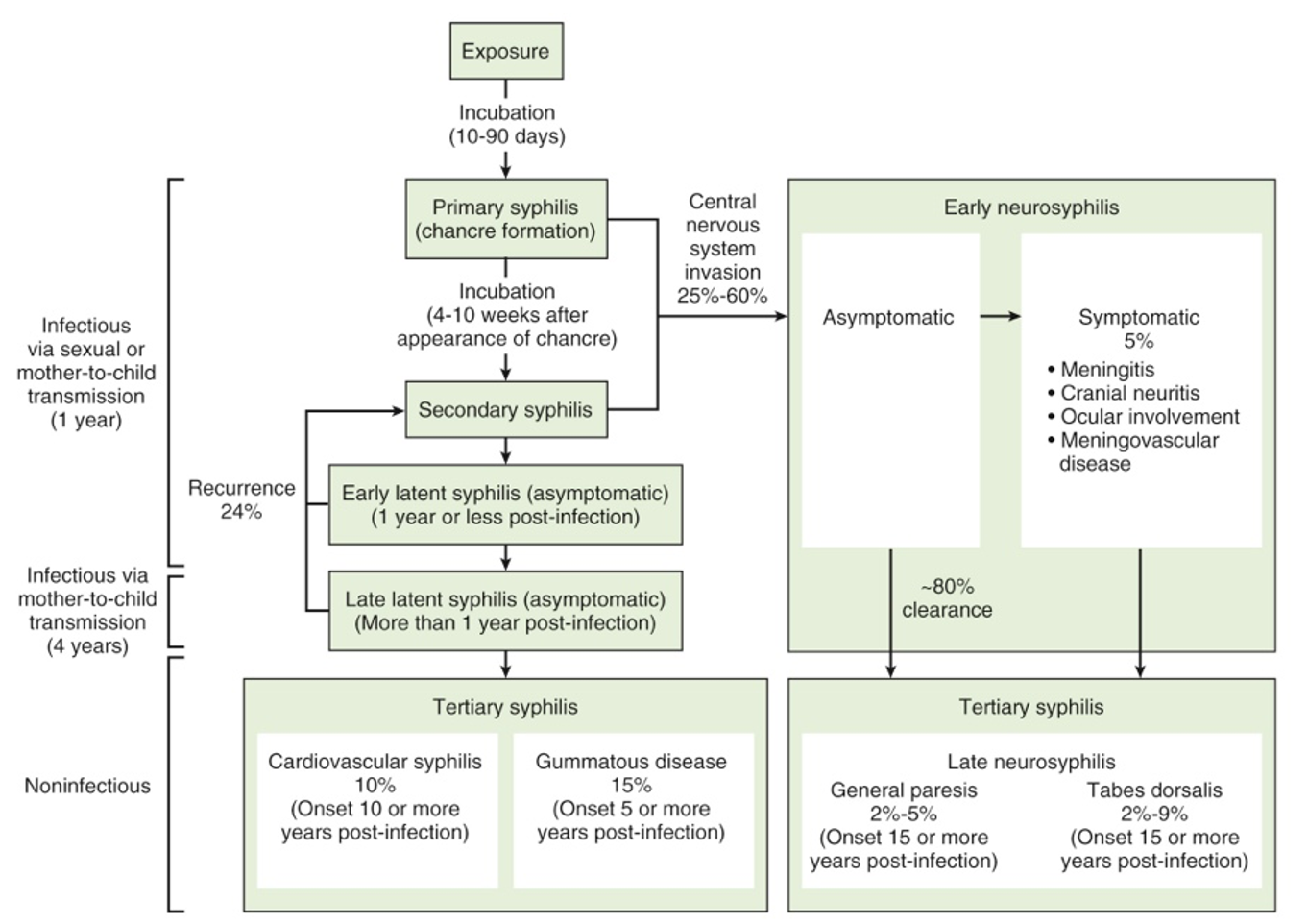
The Stages of Syphilis
- Primary Syphilis
- Painless chancre presenting in the urogenital region or oral mucosa, resolves over 4-6 weeks
- Secondary Syphilis
- Maculopapular rash (usually with palm and sole involvement) in one or more areas of the body
- Signs and symptoms: fever, swollen lymph nodes, sore throat, headaches, and other non-specific symptoms
- Latent Syphilis
- A period when there are no visible signs of symptoms
- Without treatment, syphilis will remain in the body
- Early latent syphilis is latent syphilis infection within the past 12 months
- Late latent syphilis is latent syphilis infection more than 12 months ago
- Tertiary Syphilis
- Systemic, slowly progressive, inflammatory process 10-30 years after initial infection
- Can affect the brain, nerves, eyes, heart, blood vessels, liver, bones, and joints
- Neurosyphilis, Ocular Syphilis, and Otosyphilis
- At any stage of infection, syphilis can invade the:
- nervous system (neurosyphilis)
- visual system (ocular syphilis)
- auditory and/or vestibular system (otosyphilis)
- At any stage of infection, syphilis can invade the:
Signs/symptoms of Neurosyphilis, Ocular Syphilis, and Otosyphilis (from CDC Factsheet)
Signs and symptoms of neurosyphilis can include:
- severe headache;
- trouble with muscle movements;
- muscle weakness or paralysis (not able to move certain parts of the body);
- numbness; and
- changes in mental status (trouble focusing, confusion, personality change) and/or dementia (problems with memory, thinking, and/or making decisions).
Signs and symptoms of ocular syphilis can include:
- eye pain or redness;
- floating spots in the field of vision (“floaters”);
- sensitivity to light; and
- changes in vision (blurry vision or even blindness).
Signs and symptoms of otosyphilis may include:
- hearing loss;
- ringing, buzzing, roaring, or hissing in the ears (“tinnitus”);
- balance difficulties; and
- dizziness or vertigo.

Serology
To diagnose syphilis, there are a few different tests we can order:
- Non-treponemal Tests (NTTs)
- Measure IgM & IgG with antigen binding sites that recognizes lipoidal material released from bacterium and/or dying host cells
- Rapid Plasma Reagin (titer)
- **commonly ordered especially in the hospital setting. See "Did the Treatment Work" section below for more information on how to interpret
- Treponemal Tests (TTs)
- Detection of antibodies that bind antigens specific to T. pallidum
- T. pallidum particle agglutination (TPPA)
- Fluorescent treponemal antibody
"Special note: Untreated syphilis in a pregnant person can infect their developing baby. This is why every pregnant patient should have a blood test for syphilis." (CDC Factsheet)
- Neurosyphilis, Ocular Syphilis, and Otosyphilis Mangement
- Lumbar puncture (LP) and subsequent Cerebrospinal Fluid (CSF) study
- Venereal Disease Research Laboratory (VDRL) gold diagnostic standard (NTT)

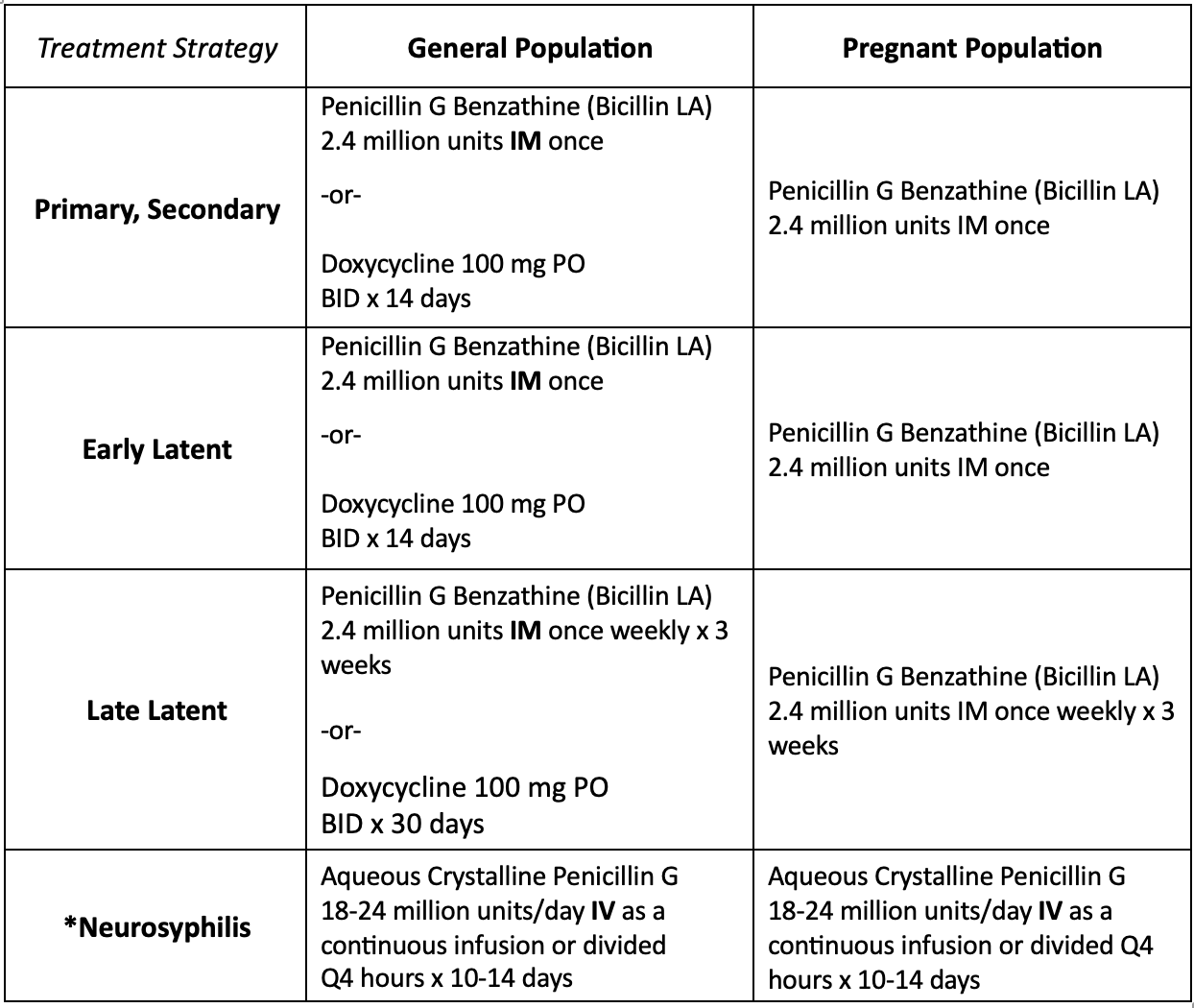
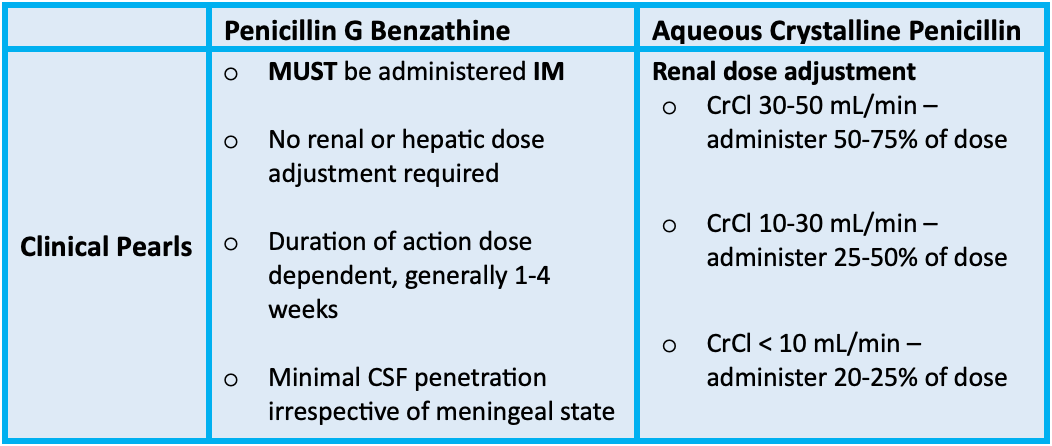
Treatment
Penicillin is our drug-of-choice for syphilis TO THIS DAY! Yes antimicrobial resistance to our approved antibiotics is a growing concern, but not with penicillin for syphilis treatment!
Doxycycline is a second-line treatment option for patients with a true hypersensitivity reaction to penicillin (and for those who cannot under go a penicillin desensitization protocol).
Disease-State Specific Clinical Pearls
- Asymptomatic neurosyphilis is always the forerunner of differential diagnoses for patients presenting with meningeal, vascular, and parenchymal syndromes
- Asymptomatic neurosyphilis during late syphilis carries a worse prognosis than asymptomatic neurosyphilis during early infection
- The likelihood of progression from asymptomatic to symptomatic neurosyphilis increases proportionally to the extent of CSF abnormalities
- If spinal fluid remains normal during the first two years of infection, or if its abnormal but reverts to normal, symptomatic neurosyphilis will not develop
Did the Treatment Work?
This section is from Kristen's clinical experience. She thought it would be beneficial to include this "hot tip" on specifically interpreting RPR Titers!
Through her own residency, Kristen learned and helped educate members of her treatment team about quantitative RPR Titers. It was pretty neat!
Both RPR and VDRL results have a quantitative titer reported. If "reactive," it will report as a ratio:
- Examples – 1:2, 1:4, 1:8, etc.
Changes in titer values are monitored after treatment to detect a therapeutic response. With adequate treatment, most individuals will return to a "non-reactive" RPR.
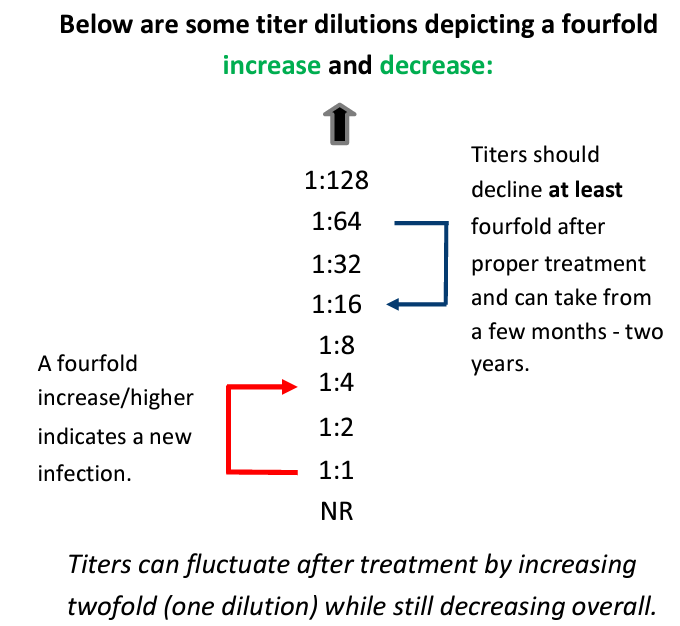
Example from a previous patient case Kristen had on service:
- A patient was admitted to the hospital and had a PMH including HIV. They were admitted with a skin and soft tissue infection. The patient also complained of a headache during admission and based on the PMH of HIV and sexual history of the patient, the team ordered an RPR Titer.
- The titer came back as Reactive! with a quantitative value of 1:16.
- The lead medical resident wanted to initiate syphilis treatment based off this result.
- Kristen went and searched the patient records to see if they had already been treated for syphilis. It turns out that two months prior, the patient was adequately treated for syphilis from an original RPR Titer of 1:64! The titer during the current hospital admission was showing a decrease in titer (1:64 down to 1:16) and the patient did not require additional treatment, as the titer did not show any signs of "re-infection."
- Kristen was able to educate her team members and save the patient additional treatment!
We hope you enjoyed today's topic discussion! Thank you, Dr. White, for you content today!
References
- Peeling RW, Mabey D, Kamb ML, Chen XS, Radolf JD, Benzaken AS. Syphilis. Nat Rev Dis Primers. 2017;3:17073. Published 2017 Oct 12. doi:10.1038/nrdp.2017.73
- Stokes JH, Beerman H, Ingraham NR: Modern Clinical Syphilology.3rd ed1944.SaundersPhiladelphia
- Kimberly A. Workowski, MD, et al. Sexually Transmitted Infections Treatment Guidelines. MMWR Recomm Rep 2021
- CDC Syphilis Fact Sheet. Last Reviewed: April 11, 2023. https://www.cdc.gov/std/syphilis/stdfact-syphilis-detailed.htm


